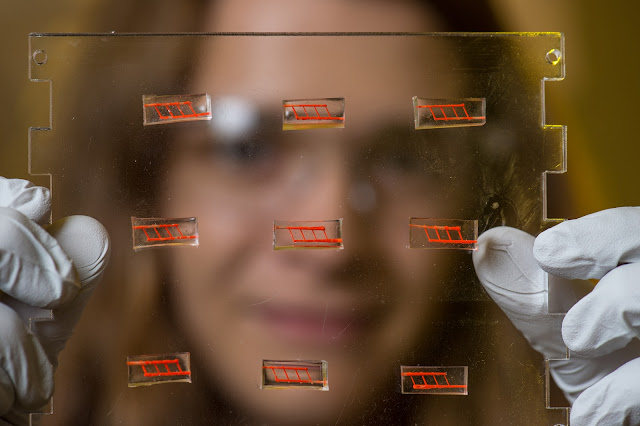
Samantha Paulsen,
a bioengineering graduate student in Jordan Miller’s lab at Rice University,
holds a plate on
which several of 3-D-printed silicone constructs have been mounted.
The constructs,
which are each about the size of a small candy gummy bear, have been
injected with red
dye to better show the network of small vessels inside. (Photo by Jeff Fitlow)
(November 3, 2015) Rice, Penn researchers create implant
with network of blood vessels
Using sugar, silicone and a 3-D printer, a team of
bioengineers at Rice University and surgeons at the University of Pennsylvania
have created an implant with an intricate network of blood vessels that points
toward a future of growing replacement tissues and organs for transplantation.
The research may provide a method to overcome one of the
biggest challenges in regenerative medicine: How to deliver oxygen and
nutrients to all cells in an artificial organ or tissue implant that takes days
or weeks to grow in the lab prior to surgery.
Using an
open-source 3-D printer that lays down individual filaments of sugar glass one
layer at a time,
the researchers “printed” a lattice of would-be blood vessels.
(Credit: Rice University)
The new study was performed by a research team led by Jordan
Miller, assistant professor of bioengineering at Rice, and Pavan Atluri,
assistant professor of surgery at Penn. The study showed that blood flowed
normally through test constructs that were surgically connected to native blood
vessels. The report was published in the journal Tissue Engineering Part C:
Methods.
Researchers at
Rice University and the University of Pennsylvania demonstrated that blood
flowed normally
through the network of small channels in the silicone construct,
which is about the
size of a small candy gummy bear. (Credit: Jordan S. Miller/Rice University)
Miller said one of the hurdles of engineering large
artificial tissues, such as livers or kidneys, is keeping the cells inside them
alive. Tissue engineers have typically relied on the body’s own ability to grow
blood vessels — for example, by implanting engineered tissue scaffolds inside
the body and waiting for blood vessels from nearby tissues to spread to the
engineered constructs. Miller said that process can take weeks, and cells deep
inside the constructs often starve or die from lack of oxygen before they’re
reached by the slow-approaching blood vessels.
From left, Jordan
Miller, Samantha Paulsen and Anderson Ta
stand with the 3-D printer they used
to create the silicone constructs.
(Credit: Jeff Fitlow/Rice University)
“We had a theory that maybe we shouldn’t be waiting,” Miller
said. “We wondered if there were a way to implant a 3-D printed construct where
we could connect host arteries directly to the construct and get perfusion
immediately. In this study, we are taking the first step toward applying an
analogy from transplant surgery to 3-D printed constructs we make in the lab.”